-
Geri Taylor enjoyed benefits from a now-abandoned Alzheimer’s medication for seven years
-
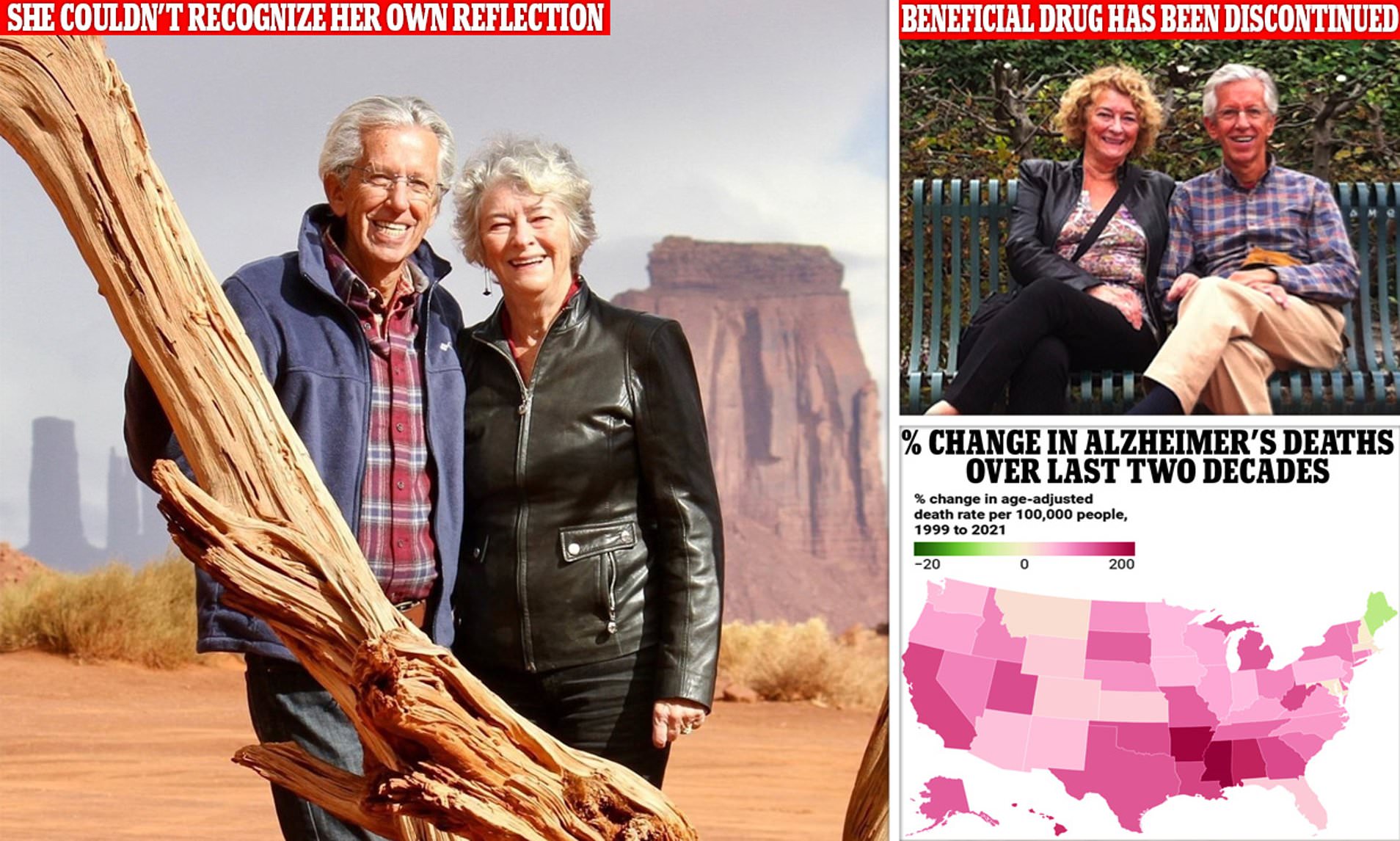
The first sign of illness emerged when she could no longer recognise her own reflection.
-
Read more: Researchers could treat Alzheimer’s disease by reversing cellular aging in the brain through a unique approach that employs a natural compound found in plants, which helps to restore youthful gene expression and promote efficient cellular renewal.
In 2012, Geri Taylor was an executive of significant stature at a substantial long-term care establishment.
New York City
As she started to exhibit noticeable indicators of mental deterioration.
At the age of 69, she experienced a lapse in memory during a business conference, and another instance, she mistakenly exited a subway at a different station and could not recall which direction led back to her residence.
One morning some time later, she was shocked when she caught sight of her reflection in the mirror, but failed to notice it was her own.
.
Research indicates that nearly eight out of 10 individuals with what is described as mild cognitive impairment (MCI) will eventually progress to develop Alzheimer’s Disease.
To Geri, it seemed only a matter of time before the other shoe would fall.
At that time, the disease had not yet reached its peak, but she felt as though she was in a state of limbo, anxiously awaiting the extent of its arrival.


Three years had passed, and Geri’s husband, Jim, was browsing newspapers one morning when he stumbled upon an article in the health section mentioning a trial for a novel treatment for cognitive impairment in its initial stages of Alzheimer’s disease.
The medication was labeled aducanumab, and its clearance through the FDA’s expedited review process was highly disputed due to a lack of robust scientific backing for its effectiveness and the potential for certain adverse reactions such as brain swelling and haemorrhaging.
After a couple met on a bus on trial held in New York City, she had also persuaded her partner to drive that morning to the distant Yale-New Haven hospital, approximately two hours away, to fill out the few remaining trial spots. Geri took one.
A particular medication, an injection containing an antibody, has been developed as a potential treatment for Alzheimer’s Disease. This medication targets the accumulation of amyloid plaque, a particular substance found in the brain that resembles sticky buildup.
Geri’s PET scans revealed significant accumulations of amyloid plaque. Alongside her deteriorating memory capabilities, this met the mandatory criteria for the study.
DNA tests suggested that Geri may have developed the condition prematurely due to genetic reasons.
She tested positive on both her maternal and paternal sides for the APOE4 gene mutation, which more than doubles the likelihood of her son developing Alzheimer’s.
Over the course of the seven-year experiment, Geri was administered a high dose of the therapeutic compound in question, whereas the placebo was withheld from her. Notably, she began to experience an improvement in her capacity for constructing coherent sentences in a relatively short period of time.
Jim told : ‘O

They embarked on a cross-country journey to deliver lectures at various churches and conferences, sharing their experiences with Alzheimer’s disease.
A network that links patients and families with healthcare providers to deliver care.
Geri always undertook half of the presentation, alternating back and forth, much like a fast-paced game of quick reflexes, where she could efficiently coordinate and manage our schedule, often requiring minimal input from me, almost negligible, over a long period of time.
That instilled both excitement and certainty in us that she was improving with the medication infusions.
At this point, Geri transformed into a socialite, passionately engaging with new acquaintances and strengthening bonds with those towards whom she felt deeply connected, living each day to the fullest as her active years unfolded.
Suddenly, the trial came to an abrupt cessation.
In March 2019, Biogen and its pharmaceutical partner Eisai jointly announced the termination of a clinical trial in which Geri was participating.
Pursuant to an interim analysis, the company decided to withdraw the drug, thus informing over 3000 Alzheimer’s patients that they would no longer receive the infusions.
Geri went completely off medication that she and her husband thought had stopped her cognitive decline for an entire year.
Jim noted, “And what caught my attention was the year she first started struggling with speech and effortless conversation. She, too, acknowledged this change, which in my perspective validated the positive effects of the medication.”
Aducanumab is a monoclonal antibody derived from cells that attach to amyloid beta, a sticky protein which occurs naturally in the brain.
In the brains of individuals with Alzheimer’s disease, an excess of precursor proteins begins to malfunction and produces abnormal amyloid beta shapes that form insoluble clusters due to this overproduction.

These aggregate formations interfere with normal neuronal activity and cellular communication pathways, ultimately leading to cell death.
Amyloid acts as a marker for Alzheimer’s disease and is a potential target for several developing medications, including aducanumab. Nevertheless, the scientific research supporting the notion that reducing amyloid can alleviate cognitive impairments is limited.”
Recent clinical trials of treatments targeting amyloid have yielded disappointing results over the past two decades, prompting debate among researchers regarding the entrenched focus on reducing amyloid levels in the quest to slow cognitive decline.
The trial resumed in 2020 and Geri could once again participate, albeit a year late; yet, due to her return, she missed an entire year of potentially beneficial treatment that could have potentially put her cognitive deterioration on hold.
This medication has been the subject of much debate and criticism since its introduction.
The June 2021 approval of the drug had sparked controversy in the past and had been subject to lengthy investigations regarding potential unethical communications between FDA personnel and the drug’s producer.
Although the drug had barely received approval, the public’s response was initially lukewarm, due in part to the hefty annual price tag of $56,000 assigned by Biogen.
Due to the fact that most individuals affected by Alzheimer’s disease are 65 years or older and are on a fixed income, coupled with the reality that Medicare, the healthcare coverage programme for seniors, is only partial in its coverage of the treatment, it proved to be out of reach for many individuals.
Earlier this year, Biogen unexpectedly discontinued the drug Aduhelm, citing that the decision was ‘not related to any safety or efficacy concerns’.
If the trial hadn’t been cut off, it is conceivable that Geri may have continued to derive advantages from the infusions.
By the time treatment resumed, Geri’s condition had deteriorated to a stage where she was unlikely to experience any improvement.
Jim stated, “Current developments in the medical field involve identifying individuals who are prone to contracting the illness before they even start demonstrating symptoms.”
‘At this point in Geri’s progression with the disease, I would say there isn’t a medication that will significantly slow down her cognitive deterioration. The medications currently being used primarily aim to manage and control symptoms, such as those associated with sundowning, rather than addressing the underlying progression of the condition.’
Geri is a full-time resident in a memory care unit. She started experiencing pronounced sundowning episodes last summer, which are characterised by confusion in the late afternoon and into the early evening.
Despite having the accomplished this from beside her continuously, Jim has however continued their work on behalf of Alzheimer’s patients and their caregivers. They established Voices of Alzheimer’s, much to the benefit of the roughly six million Americans affected by the disease.
The initial objective of the organisation was to formulate a “patient’s bill of rights”, which would assert the moral treatment required from healthcare professionals who comprehend the condition.
I recall a particularly distressing incident that prompted my advocacy for such legislation: “One time, Geri was admitted to the hospital and I was unable to be with her in her room immediately upon arrival. When I eventually arrived 30 minutes later, three caregivers were attempting to assist her in putting on a hospital gown, and she was extremely agitated.”
I found out that caregivers are not properly trained and hospitals are not equipped to identify patients suffering from dementia.
At present, Alzheimer’s does not have a definitive cure, but treatments can temporarily slow its advancement. Aduhelm was the first drug approved for Alzheimer’s in nearly two decades, prompting endorsement from the Alzheimer’s Association.
Ongoing research into new treatments will continue, and Biogen has decided to redirect its resources towards developing an alternative solution. However, donations for Alzheimer’s research currently fall short of what advocates think is necessary.
Current investment in Alzheimer’s and dementia research at the National Institutes of Health (NIH) exceeds $3.7 billion per annum, whereas the National Cancer Institute’s 2023 budget was approximately $7.3 billion.
Read more